BY: MARTY SCHLADEN
It would be a new regulation on 700,000 of Ohio’s poor, but Gov. Mike DeWine says it wouldn’t impose any additional regulatory burden on them. However, asked to describe the new requirements, the Ohio Department of Medicaid provided a lengthy document that’s full of regulations.
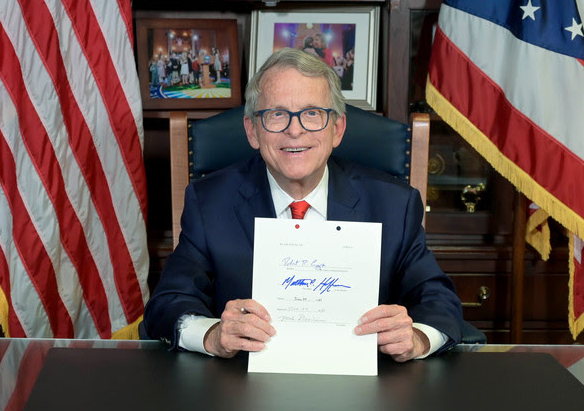
DeWine is urging Attorney General Dave Yost, a fellow Republican, to sue the federal government to allow the state to impose work requirements for able-bodied adults who are receiving Medicaid, the federal/state health program for the poor. But there are considerable reasons to wonder why that is necessary.
Former President Donald Trump granted Ohio’s request for a work requirement in 2019, but President Joe Biden rescinded the waiver before it was enacted.
DeWine’s predecessor, John Kasich, in 2014 opted into an expanded Medicaid program under the Affordable Care Act. Four years later, the portion of Ohio residents lacking health insurance had been cut in half.
Also, the state’s own research on the expansion population showed that without a work requirement, more recipients were getting work and they said Medicaid made it easier to look for and hold down a job.
It’s not hard to see why, said Loren Anthes, who leads the Cleveland-based Center for Community Solutions’ Center for Medicaid Policy.
“Medicaid is one of the most successful economic development programs that’s ever been created,” he said, describing decades of research showing that children served by the program are better off. “With Medicaid expansion, there are two strong economic benefits. Research out of Michigan showed it led to significant increases in employment in part because peoples’ basic needs were addressed. And also because things like medical debt and housing insecurity go way down.”
In other words, health coverage helps people to lead more stable lives, which makes it easier to work.
As of 2018, a full 94% of Ohio’s expansion population was either working, in school, caring for family members, or in treatment for drug addiction or other problems with physical or mental health, the Medicaid department’s analysis said.
That jibes with national research showing that most able-bodied, adult Medicaid recipients are already working.
So why is a work requirement needed? A spokeswoman for the Medicaid department implied that many recipients don’t want to work.
“Eliminating reasonable requirements discourages people from becoming self-sufficient and only reinforces government dependency,” Chief Communications Officer Lisa Lawless said in an email. “Ohio’s measured approach enables those who can, to achieve and maintain independence, and for those who cannot, to maintain a dignified quality of life with needed health care coverage. That is the central pillar of Ohio’s community engagement 1115 demonstration waiver.”
The DeWine administration hasn’t produced any evidence that the work requirements will substantially increase employment among the expansion population.
It has pointed instead to a report by the Buckeye Institute that says if people worked more, they’d earn a lot more over their lifetimes. It appears to be silent on how many more Medicaid recipients the requirements would drive into the workforce.
Because Medicaid work requirements have typically been advocated by officials who opposed the Affordable Care Act when former President Barack Obama introduced it, some have wondered, is the point of the requirements to get people working or is it just to hassle them off the system?
Indeed, the Kaiser Family Foundation reports that under an Arkansas work requirement in 2018, 18,000 — or 25% of those subject to the requirement — saw their benefits cancelled for non-compliance. Of those, just 11% were reinstated the following year.
In focus groups, people described barriers that disproportionately affect the poor. Some said they lacked access to computers and others said they moved around, making it difficult to consistently get their mail. They also said they were confused by the new layer of bureaucracy to which the state government decided to subject them.
Asked whether Ohio’s mandate would cause similar problems, DeWine’s spokesman said it wouldn’t.
“Ohio’s reasonable requirements don’t place additional administrative burdens on participants and shouldn’t be compared to other state programs as they are fundamentally different,” Press Secretary Dan Tierney said.
The requirements may be different, but the burdens seem to be quite substantial.
Asked what specific steps clients would have to take to stay in compliance with the Ohio requirements, the Medicaid department’s Lawless sent a 39-page document from the U.S. Centers for Medicare and Medicaid Services. It was loaded with bureaucratese and the page Lawless pointed to wasn’t exactly straightforward.
One of the more relevant passages said this: “After implementation of the community engagement requirement, when a beneficiary is determined eligible for Medicaid (for new applicants), or, following Medicaid eligibility renewal (for current beneficiaries) the state will notify beneficiaries of whether they are required to participate in community engagement activities as a condition of continued eligibility or whether they are exempt. Non-exempt beneficiaries will have 60 days after this notification to report their compliance with the work and community engagement requirement (and may self-attest to meeting the community engagement requirement during that time). Beneficiaries will be allowed to report compliance with the work and community engagement requirement consistent with requirements in 42 CFR 435.907(a), (such as in-person, over the phone, online, and by mail). Once the beneficiary reports one time, no further reporting is required unless the beneficiary experiences a change in circumstance consistent with 42 CFR 435.916(c).”
And while DeWine says the requirement doesn’t create new burdens, Anthes said it will place big burdens on county officials who handle benefits.
After the Ohio Legislature in 2017 passed the law creating a Medicaid work requirement, Anthes extrapolated a cost analysis by the Cuyahoga County Department of Job and Family Services. He determined that the requirement would cost county departments an additional $370 million over five years.
“As documented in other states such as Kentucky, Virginia, and Pennsylvania, 1115 Waivers with work requirements increase the administrative burden and expense of state and local governments,” the 2018 analysis says. “However, in Ohio’s application, these figures are absent from the legally-required budget neutrality estimates.”
In an interview last week, Anthes said the requirement in a way is comparable to government regulations businesses often complaining about.
“That administrative complexity means costs are going to go up because you are, in essence, creating more government — creating more regulations,” he said. “They’re just borne by individuals.”
***
Also from Ohio Capital Journal:
With gerrymandering comes strong opinions. But what is it?
The saga over drawing legislative districts in Ohio was an intense one, despite a shorter timeline in which to redraw district maps. But it’s not over yet.
With a potential court battle coming, along with a new deadline, this time for congressional districts, the concept of gerrymandering is on people’s minds.
Gerrymandering comes up every 10 years, after census data comes out and the districts that define state representatives and senators, along with Ohio’s congressional leaders, are redrawn during the redistricting process. READ MORE
Ohio Medical Board renews license of doc who claims vaccines make you magnetic
They’re forcing freedom loving Americans to choose between injection of a “deadly” vaccine or testing those who will not comply via torturing them with nasal swabs looking for a “virus that, by some claims, doesn’t even exist.”
This claim, equal parts baseless and conspiratorial, appears on a website that solicited funds to the address of a business owned by Dr. Sherri Tenpenny, a state-licensed doctor of osteopathic medicine.
Her medical license, first issued in 1984, was set to expire Oct. 1. The State Medical Board of Ohio, which credentials physicians, renewed her license Thursday for another two years.
State law allows the board, with the votes of at least six of its 12 members, to refuse renewal of any physician for “making a false, fraudulent, deceptive, or misleading statement” in relation to the practice of medicine.
This includes misrepresentation of facts that are likely to mislead, or “includes representations or implications that in reasonable probability will cause an ordinarily prudent person to misunderstand or be deceived.” READ MORE
Commentary: Jim Crow tactics reborn in Texas abortion law, deputizing citizens to enforce dubious law
The new Texas law that bans most abortions uses a method employed by Texas and other states to enforce racist Jim Crow laws in the 19th and 20th centuries that aimed to disenfranchise African Americans.
Rather than giving state officials, such as the police, the power to enforce the law, the Texas law instead allows enforcement by “any person, other than an officer or employee of a state or local governmental entity in this state.” This enforcement mechanism relies solely on citizens, rather than on government officials, to enforce the law.
This approach to enforcement is a legal end-run that privatizes a state’s enforcement of the law. By using this method of enforcement, state officials are shielded from being sued for violating the Constitution, and the law is made, at least for a time, more durable.
The U.S. Justice Department filed suit against the state on the grounds the law violated a woman’s constitutionally protected right to terminate a pregnancy before fetal viability. In its suit, the Justice Department specifically cites one of the cases that was brought over a Texas Jim Crow law that excluded Blacks from participating in primaries, which was struck down by the Supreme Court in 1944. READ MORE