A whopping 186,000 Ohioans — about 1.5% of the state’s population — tested positive for COVID-19 in November compared to about 72,000 in the prior month, according to state data.
The data is preliminary and likely an undercount given the prevalence of asymptomatic cases, the holiday week slowing down reporting from labs and local health departments, and a logjam of 7,500 antigen tests not yet reflected in Ohio Department of Health data.
Regardless of any lag, Ohio’s hospitalization load continues to surge.
More than 5,000 Ohioans were in the hospital on Monday with COVID-19, the highest active caseload of the pandemic.
“It’s a 200% increase, just since Nov. 1,” said Dr. Andy Thomas, chief medical officer for the Ohio State University Wexner Medical Center.
Thomas, speaking at a press event, said about one-third of patients in the ICU or on a ventilator statewide have COVID-19, raising the risk of their “crowding out” people in need of other medical care.
Gov. Mike DeWine said to reporters that while the data reflects an apparent slowdown in new cases, it’s unknown if the slowdown is a real decrease in transmission or a Thanksgiving-induced reporting glut.
The rate of COVID-19 deaths by day is trending upward, meanwhile, seemingly catching up to a case surge that has continued since March. More than 30 Ohioans died of COVID-19 per day, on average, in the first two weeks of November.
There’s some simple, grim calculus behind the death counts, said Dr. Mysheika Roberts, the Columbus city health commissioner.
“The more cases you have, the more deaths you’re going to have,” she said.
Dr. Bill Miller, an infectious disease expert at Ohio State University, said the rise in deaths is to be expected and linked to the rise in new cases.
On a positive note, he said the death rate is lower than what you might expect given the rise of cases.
“Part of that may be that clinicians’ have gotten better at treating it,” he said. “Another part is that we have, generally, fewer cases among older folks than we did in the spring.”
At his press conferences, DeWine has increasingly ceded the floor to nurses and physicians to relay what they’re seeing behind hospital walls.
While he avoided mention of any new health orders to slow down the virus, he struck a dire tone and urged Ohioans to “pull back” on things like travel and social gatherings.
“There’s no indication we plateaued out yet, no indication at all, and even if we did plateau out at this level, it’s still an exceedingly high level,” he said.
Under the Public Health Advisory System, a composite of seven measurements like infection rates and medical visits, the vast majority of Ohio counties are red (“very high levels of exposure and spread”) and a record four are now purple (“severe levels of exposure and spread”): Franklin, Lake, Montgomery and Lorain.
Franklin County Health Commissioner Joe Mazzola said in an interview Monday the state is in a tight spot right now. He’s expecting some kind of bloom of Thanksgiving cases, but hopeful it isn’t overpowering.
Regardless, it has been a tough month.
“We have seen just an explosion of new cases across our community,” he said.
Dan Suffoletto, a public information officer at Public Health Dayton and Montgomery County, said it’s too early right now to tell if there’s a Thanksgiving surge on the horizon.
“We don’t know,” he said. “It’s a 14-day incubation period, so that remains to be seen.”
***
Also from Ohio Capital Journal:
Becker files articles of impeachment against DeWine for COVID-19 response
When state Rep. John Becker’s summer plan to impeach Gov. Mike DeWine received quick endorsements from three legislative colleagues, he hoped the momentum would snowball throughout the end of 2020.
That did not happen. In social media posts and Statehouse speeches, Republican lawmakers have criticized the governor’s handling of COVID-19. They’ve complained about a lack of communication and the need for constitutional checks and balances.
But they evidently do not want to impeach him. No one else has publicly supported the effort since it was announced in August. READ MORE
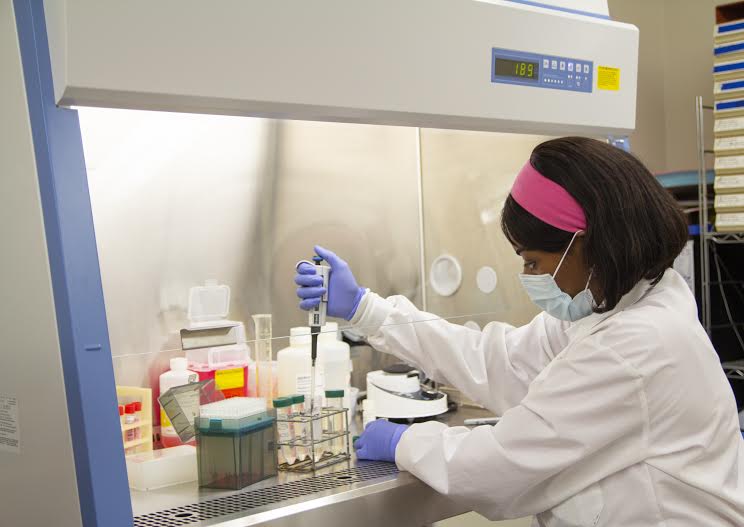
Rural hospitals are under siege from COVID-19 – here’s what doctors are facing, in their own words
It’s difficult to put into words how hard COVID-19 is hitting rural America’s hospitals. North Dakota has so many cases, it’s allowing asymptomatic COVID-19-positive nurses to continue caring for patients to keep the hospitals staffed. Iowa and South Dakota have teetered on the edge of running out of hospital capacity.
Yet in many communities, the initial cooperation and goodwill seen early in the pandemic have given way to COVID-19 fatigue and anger, making it hard to implement and enforce public health measures, like wearing face masks, that can reduce the disease’s spread.
Rural health care systems entered the pandemic in already precarious financial positions. Over the years, shifting demographics, declining revenue and increasing operating expenses have made it harder for rural hospitals to stay in business. The pandemic has made it even more difficult. In mid-March, most rural hospitals halted elective procedures to slow the spread of the virus, cutting their revenue further, and many have faced price gouging for supplies given extreme shortages. READ MORE
HELP OHIO CAPITAL JOURNAL GROW Make a tax-deductible donation